4 TYPES OF CHOLESTEROL THAT AFFECT YOUR HEART HEALTH (AND WHAT TO DO ABOUT THEM)
When you think about cholesterol—if you think about it at all—your mind probably jumps to its effect on your heart disease risk, particularly if your doctor has said your levels aren’t where they should be.
It’s more than a little anxiety-inducing when blood test results come back with a laundry list of terms—LDL, HDL, triglycerides—followed by hard-to-interpret numbers. What does it all mean?
Here’s the thing: Cholesterol is both good and bad when it comes to your health, depending on where it is in your body, how much there is, and what kind it is. Here’s a rundown of the different types of cholesterol and what you should know about each.
First, what is cholesterol?
Cholesterol is a waxy fat that’s churned out by your liver. It gets paired with proteins and hitches a ride on them so it can get ferried throughout your bloodstream.
Despite its bad rap, cholesterol plays a vital role in your health, according to cardiologist Nieca Goldberg, MD, medical director of Atria New York City and a clinical associate professor at NYU Grossman School of Medicine. Your body uses cholesterol to make cells, certain hormones, and the bile used to digest food, among other things.1
But not all cholesterol is the same. Depending on the proteins it’s paired with—known scientifically as lipoproteins—cholesterol might get dropped off, picked up, or otherwise handled in ways that might affect your health as it travels through your blood vessels.
Knowing your lipoprotein situation can give you some insight into what’s happening inside your body—and help you sort out what those cholesterol test results mean.
Low-density lipoprotein or LDL (a.k.a. “bad cholesterol”)
Since you need cholesterol, calling LDL “bad” is overly simplistic. But this is one type of cholesterol that you want to have less of, Dr. Goldberg says, because it can contribute to clogging your arteries, which increases your risk of heart disease.
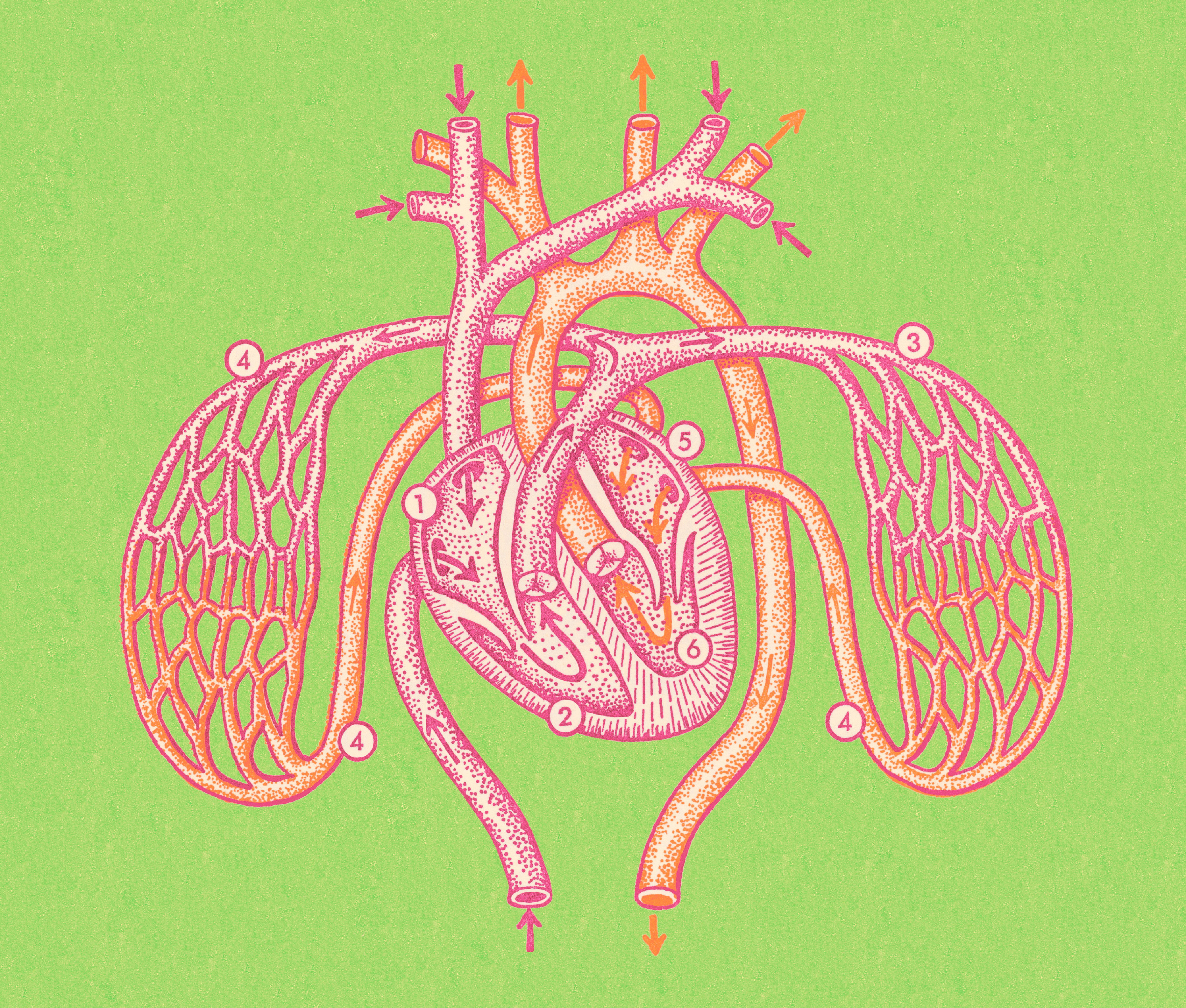
When your body has too much LDL, cholesterol can be deposited in places you don’t want it, like your blood vessels (including the ones leading to your heart). This can contribute to a waxy buildup of plaque that makes your arteries narrow and stiff, also known as atherosclerosis. Most of the time, this process causes no symptoms at all. That’s why doctors recommend that generally “healthy” adults get routine blood tests for cholesterol every four to six years, and more often only if you have diabetes, heart disease, or a family history of high cholesterol.
That said, atherosclerosis—which affects about 50% of adults over the age of 45 in the US—slows blood flow to the heart (as well as other organs and tissues), and if a plaque bursts, a blood clot can form and trigger a heart attack. Things don’t always get to this dire stage but, “sometimes the first sign that something’s wrong is a heart attack,” Guy Mintz, MD, the director of cardiovascular health and lipidology at North Shore University Hospital, in Manhasset, New York, tells SELF.
LDL, Dr. Mintz stresses, is only one reason you can develop clogged arteries: High blood pressure and blood sugar can also do a number on your blood vessels. Just as you can improve those health markers through lifestyle changes, you also have some control over your LDL. Your levels tend to go up when you smoke, don’t get regular exercise, and eat a lot of processed and commercially prepared foods, which tend to be high in saturated or trans fats that can potentially up your heart disease risk.
So how low should your LDL be? In general, you’re doing well if your blood test for cholesterol (also known as a lipid panel) comes back with an LDL reading below 100 mg/dL, per the National Library of Medicine. If you’ve had a heart attack or stroke in the past, and you’ve been prescribed some kind of cholesterol-lowering medication, your doctor might want to see it below 70 mg/dL. Why? Some research suggests that an even lower number is beneficial for those who already have heart disease.2
High-density lipoprotein or HDL (a.k.a. “good cholesterol”)
This type is considered heart-friendly. That’s because HDL absorbs extra cholesterol, taking it back to your liver to be flushed out of your body, which helps prevent it from clogging up your arteries. (The liver uses the cholesterol to make bile and then it exits your body via your poop.) 3
So in this case, a higher number is better. The general advice: People assigned female at birth should aim to keep their HDL at or above 50 mg/dL, while those assigned male at birth should aim for at or above 40 mg/dL.
If you get an HDL reading that’s lower than that, it might be due to some of the same factors that boost LDL, like smoking cigarettes or not getting enough movement each day. Other potential contributors to a low reading include conditions like type 2 diabetes and medications like beta-blockers, which are used to lower blood pressure.4
Dr. Mintz stresses that having a healthy HDL level does not mean you can ignore your LDL levels—you want both to be in the recommended range for optimal heart health.
Very low-density lipoprotein (VLDL) cholesterol
VLDL (or very low-density lipoprotein) is a less well-known relative of LDL. It matters because it’s the primary ride for triglycerides, a type of fat in the blood that is used for energy. Triglycerides are the most abundant type of fat in your body, per the National Library of Medicine. Their job is to store excess calories from the foods you eat.
A combo of elevated VLDL and high triglycerides is bad news for your heart. That’s why when you get a lipid panel, you will see triglycerides listed along with your total cholesterol, LDL, and HDL. Ideally, your triglycerides should be below 150 mg/dL.
Some lifestyle factors—like primarily eating foods that are high in added sugar or saturated fat—can raise your triglycerides. So can drinking too much alcohol, certain conditions like thyroid disease, and the same lifestyle factors that increase LDL and lower HDL.
Lipoprotein (a)
Researchers have only recently started to zero in on lipoprotein (a). It appears to be another bad guy under the cholesterol umbrella, according to Anurag Mehta, MD, the director of preventive cardiology at VCU Health’s Pauley Heart Center in Richmond, Virginia. But there’s still a lot that experts don’t know about it.
Lp(a) appears to be mostly determined by genetics, and Dr. Mehta says scientists aren’t sure what functions it serves in the body, exactly. Nor is there universal agreement on what constitutes as “high” Lp(a), however, general guidelines point to 50 mg/dL as the threshold.
Lp(a) is not part of the standard lipid panel, Dr. Mehta notes. Testing is recommended only for people with known atherosclerosis-related disease or a family history of premature heart disease or stroke since higher Lp(a) levels have the potential to impact these folks the most.5
You can’t move the needle on Lp(a) with lifestyle changes, unfortunately. (Researchers are studying potential medication options to see if they make a difference.) But if you know you have a higher risk of heart disease and your Lp(a) levels are high, Dr. Mehta says you should still try to change the things you do have some control over, like lowering your LDL if it’s high, as well as keeping your blood pressure and blood sugar in check.
What you can do about all this
First, get your standard lipid panel, which you can ask your doctor about during an annual physical. Dr. Goldberg says it’s recommended for anyone who is at least 20 years old, and your health care provider will let you know how frequently you should be tested.
If you can, you should also try to find out whether any of your close relatives have had cardiovascular disease, Dr. Mehta says. That gives your doctor a better picture of your overall risk. (Here’s a guide on how to talk to your family about their heart health history.)
A heart-healthy eating plan can go a long way to improve your LDL, HDL, and triglyceride levels in one fell swoop. Dr. Goldberg recommends loading your plate with fruits and vegetables, legumes, fiber-rich grains, fish and poultry, and unsaturated fats from sources like nuts and seeds. (We even have recipe inspo for you!)
And find a type of movement you genuinely enjoy. Regular aerobic exercise, like walking or running, can improve your LDL and HDL levels—as well as your cardiovascular fitness. Aim for 150 minutes of moderately intense cardio spread throughout the week.
If you’re younger than 40, lifestyle changes are likely all that you’ll need to get back on track if your numbers aren’t ideal (unless your LDL is very high—190 mg/dL or above). If you’re 40 or older, your doctor might recommend cholesterol-lowering medication if you have a high risk of heart disease.
Annual visits with your primary care doc are important too. That’s partly to get a picture of your “overall health status,” Dr. Goldberg points out. But when it comes to your cholesterol, a routine screening is the only way to know where you stand.
As Dr. Mehta stresses: “You’ll never know if you have high cholesterol by how you feel.”
Sources:
- Nutrients, New Insights Into Cholesterol Functions: A Friend or an Enemy?
- JAMA Cardiology, Efficacy and Safety of Further Lowering of Low-Density Lipoprotein Cholesterol in Patients Starting With Very Low Levels
- Advances in Clinical Chemistry, Role of ATP-Binding Cassette Transporters A1 and G1 in Reverse Cholesterol Transport and Atherosclerosis
- Clinical Cardiology, The Effects of Beta-Adrenergic Blocking Agents on Blood Lipid Levels
- American College of Cardiology, An Update on Lipoprotein(a): The Latest on Testing, Treatment, and Guideline Recommendations
Related: